“Just Gingivitis”
So many people think it’s natural and normal for their gums to bleed. “I know I’m cleaning really well if I can make my gums bleed.” “Oh, it’s just gingivitis.” And to that I have to ask, Do your elbows bleed when you take a shower? Well, they shouldn’t, and neither should the gums.
Bleeding gums represent an open wound in one of the most contaminated parts of the body, bar none.
And beyond bad breath there are a whole slew of effects on the whole rest of the body as the bacteria and bacterial waste-products seep down into the rest of the system: heart, blood vessels, lungs, kidneys, brain, reproductive organs, joints, etc., etc….
Some of these things can be deadly.
If the direct effects are not bad enough, there are secondary inflammatory stimulatory effects on the immune system, and these effects can lead to wide-ranging damage.
Some of the targets and diseases are listed below. Click next to them to read in more depth.
Please contact us if you have contributions to this site or questions: CLICK HERE TO EMAIL ZT4BG
“Just Gingivitis” 
Clearly, this picture from Walter Loesche is WAY beyond gingivitis.
But one can easily see the tremendous surface area of raw, exposed connective tissue and its associated vasculature, a pathway directly into the circulation. This is frank periodontitis. Gingivitis is much more subtle and hard to notice but can represent another great source of ingress into the bloodstream.
Click on the blue categories below to get much more detail in each subject area:
-
Cardiovascular disease
-
Diabetes
-
Pre-term/low birthweight babies
-
Cerebrovascular disease/Stroke
-
Cancer
-
Joint disease/arthritis
-
What can we DO about it?
Some General Articles
Read the pdf’s:
Periodontal Infection and Glycemic Control in Diabetes: Current Evidence
Diagnostic and Therapeutic Strategies for the Management of the Diabetic Patient
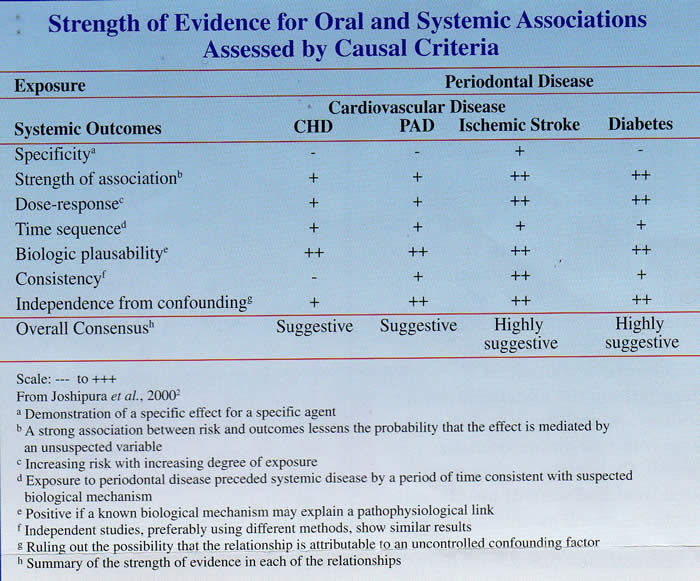
Strength of Evidence Relating Periodontal Disease and Cardiovascular Disease
Infection or Inflammation: The Link Between Periodontal Disease and Systemic Disease
Oral Health – General Health Interrelationships: Health Policy Implications
For a nice interactive online overview course on the oral/systemic links, visit PerioEducation. com CLICK HERE
Dentists: also worth visiting the Diamond Age Systems pages for more resources and information: CLICK HERE
Chronic Inflammation in Periodontal Diseases: Immunopathogenesis and Treatment
Inflammatory burden is CUMULATIVE.
To read the whole article: CLICK HERE
Preventing Hospital Pneumonias: Brush the Teeth
ScienceDaily (Dec. 15, 2008) — Hospital-borne infections are a serious risk of a long-term hospital stay, and ventilator-associated pneumonia (VAP), a lung infection that
develops in about 15% of all people who are ventilated, is among the most dangerous.
With weakened immune systems and a higher resistance to antibiotics, patients who rely
on a mechanical ventilator can easily develop serious infections — as 26,000 Americans do every year.
Thanks to a proven new clinical approach developed by Tel Aviv University nurses, though, there is a new tool for stopping the onset of VAP in hospitals.
This new high-tech tool? An ordinary toothbrush.
Three Times a Day Keeps Pneumonia Away
“Pneumonia is a big problem in hospitals everywhere, even in the developed world,” says Nurse Ofra Raanan, the chief researcher in the new study and a lecturer at Tel Aviv
University’s Department of Nursing. “Patients who are intubated can be contaminated with pneumonia only 2 or 3 days after the tube is put in place. But pneumonia can be
effectively prevented if the right measures are taken.”
Raanan, who works at the Sheba Academic School of Nursing at The Chaim Sheba Medical Center, collaborated with a team of nurses at major medical centers around Israel. The nurses found that if patients — even unconscious ones — have their teeth brushed three times a day, the onset of pneumonia can be reduced by as much as 50%.
A Pioneering Study with Measurable Effects
It’s difficult to quantify the effects precisely, the researchers say. “While the research shows a definite improvement in reducing the incidence of hospital-borne pneumonia, it’s hard to say by exactly how much toothbrushing prevents VAP,” says Raanan, but the published evidence shows a direct correlation for intubated patients.
“Sometimes, however, doctors and nurses do everything right and the patient still gets
pneumonia. But this approach will certainly improve the odds for survival.”
Normally, the teeth and oral cavity in a healthy mouth maintain a colony of otherwise
harmless bacteria. Infection takes root when a breathing tube allows free passage of the
“good” bacteria into the lower parts of the lung. The bacteria travel in small water
droplets through the tube and colonize the lung. Once there, the bacteria take
advantage of a patient’s weakened immune system and multiply. A regular toothbrushing
kills the growth and subsequent spread of the bacterium that leads to VAP.
Augmenting the Preventative Routine
There are additional steps for preventing the onset of VAP. Today, nurses typically use a
mechanical suction device to remove secretions from the mouth and throat. They also put patients in a seated position and change the position every few hours. Toothbrushing, say Tel Aviv University nurses, should be added to the routine.
Although nurses in some American hospitals already practice toothbrushing on ventilated
patients, these new results may convince medical centers around the world to invest more resources in this routine practice, thereby saving lives.
How to avoid heart disease: brush your teeth, say scientists
by Marlowe HoodWed Sep 10, 7:16 PM ET
Here’s another reason to brush your teeth: poor dental hygiene boosts the risk of heart attacks and strokes, a pair of studies reported this week.
Heart disease is the number one killer worldwide, claiming upward of 17 million lives every year, according to the World Health Organization.
Smoking, obesity and high cholesterol are the most common culprits, but the new research shows that neglected gums can be added to the list.
“We now recognize that bacterial infections are an independent risk factor for heart diseases,” said Howard Jenkins of the University of Bristol in Britain, at a meeting of the Society for General Microbiology in Dublin.
“In other words, it doesn’t matter how fit, slim or healthy you are, you’re adding to your chances of getting heart disease by having bad teeth,” the professor said.
There are up to 700 different bacteria in the human mouth, and failing to scrub one’s pearly whites helps those germs to flourish.
Most are benign, and some are essential to good health. But a few can trigger a biological cascade leading to diseases of the arteries linked to heart attacks and stroke, according to the new research.
“The mouth is probably the dirtiest place in the human body,” Steve Kerrigan of the Royal College of Surgeons in Dublin said.
“If you have an open blood vessel from bleeding gums, bacteria will gain entry to your bloodstream.”
Once inside the blood, certain bacteria stick onto cells called platelets, causing them to clot inside the vessel and thus decreasing blood flow to the heart.
“We mimicked the pressure inside the blood vessels and in the heart, and demonstrated that bacteria use different mechanisms to cause platelets to clump together, allowing them to completely encase the bacteria,” he said.
This not only created conditions that can provoke heart attacks and strokes, it also shielded the bacteria from both, immune system cells and antibiotics.
“These findings suggest why antibiotics do not always work in the treatment of infectious heart disease,” Jenkins said.
In separate research, a team led by Greg Seymour of the University of Otago Dunedin in New Zealand showed how other bacteria from the mouth can provoke atherosclerosis, a disease that causes hardening of the arteries.
All organisms — including humans and bacteria — produce “stress proteins,” molecules produced by conditions such as inflammation, toxins, starvation, or oxygen deprivation.
One function of stress proteins is to guide other proteins across cell membranes.
But they can also can latch onto foreign objects, called antigens, and deliver then to immune cells, provoking an immune reactions in the body.
Normally, the body does not attack its own stress proteins.
But bacterial stress proteins — which are similar — do trigger a response, and once that has happened the immune system can no longer differentiate between the two, said Seymour.
“White blood cells can build up in the tissue of arteries, causing atherosclerosis,” he explained in a phone interview.
Copyright © 2008 Agence France Presse
Clin Microbiol Infect. 2007 Oct;13 Suppl 4:3-10
Relationship between periodontal infections and systemic disease.
Seymour GJ, Ford PJ, Cullinan MP, Leishman S, Yamazaki K.
Faculty of Dentistry, University of Otago, Dunedin, New Zealand. [email protected]
Oral conditions such as gingivitis and chronic periodontitis are found worldwide and are among the most prevalent microbial diseases of mankind. The cause of these common inflammatory conditions is the complex microbiota found as dental plaque, a complex microbial biofilm. Despite 3000 years of history demonstrating the influence of oral status on general health, it is only in recent decades that the association between periodontal diseases and systemic conditions such as coronary heart disease and stroke, and a higher risk of preterm low birth-weight babies, has been realised. Similarly, recognition of the threats posed by periodontal diseases to individuals with chronic diseases such as diabetes, respiratory diseases and osteoporosis is relatively recent. Despite these epidemiological associations, the mechanisms for the various relationships remain unknown. Nevertheless, a number of hypotheses have been postulated, including common susceptibility, systemic inflammation with increased circulating cytokines and mediators, direct infection and cross-reactivity or molecular mimicry between bacterial antigens and self-antigens. With respect to the latter, cross-reactive antibodies and T-cells between self heat-shock proteins (HSPs) and Porphyromonas gingivalis GroEL have been demonstrated in the peripheral blood of patients with atherosclerosis as well as in the atherosclerotic plaques themselves. In addition, P. gingivalis infection has been shown to enhance the development and progression of atherosclerosis in apoE-deficient mice. From these data, it is clear that oral infection may represent a significant risk-factor for systemic diseases, and hence the control of oral disease is essential in the prevention and management of these systemic conditions.
Journal of Periodontology January 2002, Vol. 73, No. 1, Pages 73-78 (doi:10.1902/jop.2002.73.1.73)
Systemic Release of Endotoxins Induced by Gentle Mastication: Association With Periodontitis Severity Sabine O. Geerts
Background: Periodontitis has recently been identified as a potential risk factor for systemic pathologies such as cardiovascular disease, the hypothesis being that periodontal pockets could release pro-inflammatory bacterial components, for instance endotoxins, into the bloodstream. It is known that the oral cavity can be a source of circulating bacteria, but this has never been shown for bacterial endotoxins, and no evidence exists so far that the risk of systemic injury is related to the severity of periodontitis. The aim of the present study was to test the influence of gentle mastication on the occurrence of endotoxemia in patients with or without periodontal disease.
Methods: A total of 67 subjects were periodontally examined and grouped according to their periodontal status. This classification was based on an original index of severity of periodontal disease (periodontal index for risk of infectiousness, PIRI) aimed at reflecting the individual risk of systemic injury from the periodontal niches. Thus, the patients were classified into 3 risk groups: low, PIRI = 0; n = 25; moderate, 1 ≤PIRI ≤5, n = 27; and high 6 ≤PIRI ≤10, n = 15. Blood samples were collected before and 5 to 10 minutes after a standardized session of gentle mastication for detection of circulating endotoxins. Blood samples were tested with a chromogenic limulus amoebocyte lysate assay.
Results: Overall, blood levels of endotoxin after mastication were found to be significantly higher than before mastication (0.89 ± 3.3 pg/ml versus 3.0 ± 5.8 pg/ml; P = 0.0002). Likewise, the incidence of positive endotoxemia rose from 6% before mastication to 24% after mastication (P = 0.001). When accounting for the PIRI index, endotoxin levels and positive endotoxemia proved to be significantly higher in patients with severe periodontal disease than in the subjects with low or moderate periodontitis.
Conclusions: Gentle mastication is able to induce the release of bacterial endotoxins from oral origin into the bloodstream, especially when patients have severe periodontal disease. This finding suggests that a diseased periodontium can be a major and underestimated source of chronic, or even permanent, release of bacterial pro-inflammatory components into the bloodstream.
Mouth-Body Connection
 |
Bacteria associated with periodontal disease have been linked to other serious health risks.
|
In July of 1998, the American Academy of Periodontology launched an effort to educate the public about new findings which support what dental professionals had long suspected: Infections in the mouth can play havoc elsewhere in the body.
Since July of 1998, evidence has continued to mount to support these links. While more research needs to be done to say definitively that people with periodontal disease are at higher risk for developing heart disease, stroke, uncontrolled diabetes, preterm births and respiratory disease, periodontists do know that periodontal disease is a bacterial infection, and all infections are cause for concern.
Periodontal bacteria can enter the blood stream and travel to major organs and begin new infections. Research is suggesting that this may:
- Contribute to the development of heart disease, the nation’s leading cause of death.
- Increase the risk of stroke.
- Increase a woman’s risk of having a preterm, low birthweight baby.
- Pose a serious threat to people whose health is compromised by diabetes, respiratory diseases, or osteoporosis.
-
Aetna and Columbia Announce Results from Study Showing Relationship between Periodontal Treatment and a Reduction in the Overall Cost of Care for Three Chronic Conditions
3/20/2006 10:03:00 AM EST
Aetna (NYSE:AET) and Columbia University College of Dental Medicine conducted a study that found a relationship between periodontal (gum) treatment and the overall cost of care for several chronic diseases. The results of the study, which included approximately 145,000 Aetna members with continuous dental and medical coverage, indicate that periodontal care appears to have a positive effect on the cost of medical care, with earlier treatment resulting in lower medical costs for members with diabetes, coronary artery disease (CAD), and cerebrovascular disease (CVD) or stroke.
“The results of this study are encouraging because they show the connection between good oral health and overall well-being, as well as illustrating that the early treatment of periodontal disease can help reduce medical costs for these conditions,” said Pat Farrell, head of Aetna Specialty Products. “We believe that in addition to lowering medical costs, we are also helping to improve members’ quality of life. We will continue to work with Columbia to demonstrate ways that dental care can improve the overall health of our members.”
“Systemic health is often associated with the condition of the oral cavity in that many systemic diseases manifest in the mouth; however, less is known about the connection between a diseased periodontium and the impact it may have on systemic health,” said David A. Albert, D.D.S., M.P.H., Associate Professor of Dentistry at Columbia University. “The association between periodontal infection and systemic health has important implications for the treatment and management of patients.”
The retrospective study of claims data included an examination of approximately 145,000 members participating in Aetna PPO plans with continuous dental and medical coverage over two years. Periodontal care appeared to have a positive effect on the cost of medical care in this two-year study (2001, 2002), with earlier treatment resulting in lower medical costs for diabetes, CVD and CAD. In addition, the actual cost of medical care for patients with diabetes and CAD was found to be lower if they received periodontal care in the first year of the study.
About Columbia University College of Dental Medicine
Since its inception in 1852 and its incorporation into Columbia University in 1917, the College of Dental Medicine has vigorously pursued its commitment to education, patient care and research. Recognizing the value to the public and the dental specialties, the college established the first formal specialty education program in orthodontics in the 1920s. Columbia went on to establish programs in periodontics, endodontics, oral/maxillofacial surgery, prosthodontics, pediatric dentistry and advanced programs. The college provides general dentistry, oral surgery, pediatric dentistry, orthodontics, and other clinic services to many members of the community through its Faculty Practice, Postgraduate and Specialty Practice, and Undergraduate Clinic. Columbia encourages and supports all forms of academic research efforts that have direct impact on improving oral health by fostering faculty and student participation in research and training students in current research methodologies.
www.aetna.com.
-
ScienceDaily (Nov. 28, 2007) — A new study found that prevention of periodontal diseases may lead to savings on not only dental costs, but also medical care costs. Periodontal, or gum diseases have been linked to systemic health conditions including diabetes, cardiovascular disease, and respiratory problems.
The study, conducted in Japan, examined the effect of periodontal diseases on medical and dental costs in 4,285 patients over a 3.5 year time span. The patients were between the ages of 40-59. Researchers found that cumulative health care costs were 21% higher for those patients with severe periodontal disease than those with no periodontal
disease. Severe periodontal disease, or periodontitis, involves bone loss and diminished attachment around the teeth.“While previous studies have evaluated the potential link between periodontal diseases
and other systemic conditions, this study provides an interesting analysis of total health care costs and the financial impact of having periodontal diseases,” explained JOP
editor Kenneth Kornman, DDS. “The research suggests that patients with sever periodontal diseases incur higher overall health care expenses as compared to those patients with no periodontal disease. Prevention of periodontal disease may be very important in overall health, and this study suggests that it may also indirectly translate into lower total health care costs.”“Everyone is looking for ways to reduce health care costs,” said Susan Karabin, DDS,
President of the American Academy of Periodontology. “Especially those who are in
an age category where they are more susceptible to periodontal diseases. Because
of the relationship between the mouth and the rest of the body, treating periodontal
disease may be one simple way to decrease total health care costs. If caught early,
periodontal diseases can be treated using simple non-surgical techniques which can
restore your mouth to a healthy state.”Journal of Periodontology article: “The effect of periodontal disease on medical and
dental costs in a middle-aged Japanese population: A longitudinal worksite study,”
November 2007. -
-
Severe periodontitis is associated with systemic inflammation and a dysmetabolic status: a case-control study Authors: Nibali, Luigi1; D’Aiuto, Francesco1; Griffiths, Gareth; Patel, Kalpesh1; Suvan, Jean1; Tonetti, Maurizio S.2
Source: Journal of Clinical Periodontology, Volume 34, Number 11, November 2007 , pp. 931-937(7)
bstract Background and Aim: A cluster of metabolic factors defines a syndrome that predisposes to diabetes and cardiovascular disease. Chronic infections such as periodontitis might alter these individual metabolic factors and the systemic inflammatory burden. The aim of this study was to investigate the association between severe periodontitis and increase in inflammatory and metabolic risk factors for cardiovascular disease. Materials and Methods: We examined 302 patients with severe periodontitis and 183 healthy controls, and we collected a blood sample from each subject in order to investigate differences in inflammatory (leukocyte numbers and differential counts) and metabolic markers (lipids and glucose). Results: After correcting for differences in age, gender, smoking and ethnicity, periodontitis subjects exhibited a low-grade systemic inflammation (increased white cell counts, 1.10±1.02 × 109/l, 95%CI 1.05-1.15, p=0.0001), dyslipidemia [lower high-density lipoprotein cholesterol, 1.14±1.03 mmol/l, 95%CI 1.08-1.20, p<0.0001 and higher low-density lipoprotein cholesterol, 1.12±1.03, 95%CI 1.05-1.19, p<0.0001) and increased non-fasting serum glucose levels (1.04±1.01 mmol/l, 95%CI 1.02-1.06, p=0.01) when compared with controls. The associations were confirmed in a subpopulation of Caucasian non-smokers. A trend for a dose dependent effect of the number of periodontal pockets on the tested inflammatory and metabolic markers was observed. Conclusions: These data suggest a possible link between severe generalized periodontitis, systemic inflammation and a dysmetabolic state in otherwise healthy individuals.
-
For several good articles on the oral/systemic link, take a look at the Colgate dental site. CLICK HERE
And, from the CDC: the 2003 Bethesda conference on the oral/systemic link. Not the most up-to-date, but much material here to explore:
- Introduction to Periodontal Diseases: Clinical Presentations, Etiology, and Pathogenesis
- Population Aspects, Smoking, and Other Modifiable Risk Factors for Periodontal Disease
- Genetic Aspects of Periodontal Diseases
- Periodontal Diseases and Respiratory InfectionsPeriodontis and Cardiovascular Disease
- The Inflammatory Link between Periodontitis and Cardiovascular Diseases
- Periodontitis and Cardiovascular Diseases – Comorbid Conditions?
- Difficulties in Evaluating the Relationships Between Periodontal Disease and Cardiovascular Diseases
- Potential Public Health Implications of Periodontal Disease and Cardiovascular Disease RelationshipsDiabetes and Periodontal Disease
- Diabetes and Periodontal Disease: Current Concepts
- Diabetes and Periodontal Disease: Important Gaps in Knowledge and Methodological Issues
- Diabetes and Its Complications: Designing New Therapies for this EpidemicPeriodontal Disease and Reproductive Outcomes
- Potential Impact of Maternal Periodontitis on Reproductive Outcomes
- Periodontal Disease as a Risk Factor for Preterm Birth: Epidemiology and a Pilot Intervention Study
- Potential Public Health Implications of Associations Between Periodontitis and Reproductive Outcomes
-
Another related site: The Oral Physician http://www.theoralphysician.com/
Dr. Randall LaFrom has put together a great deal of useful information
Medical Conditions:
Cardiovascular Disease – (Circulatory Vessel Diseases – Heart Attack, Stroke, etc.)
Diabetes – (Insulin imbalance in from the pancreas)
Kidney Disease
Pregnancy
Respiratory Disease – (COPD, Emphysema, Bronchitis)
Sleep Apnea – (Obstructive Sleep Apnea, Snoring)Dental Conditions:
Dental Caries
Periodontal Disease
Sleep Apnea – (Obstructive Sleep Apnea, Snoring)Vitamins, Foods, Herbs, and Supplements:
Fluoride
Nutrition – (foods and drinks, i.e. Green tea)
XylitolLifestyle:
Alcohol Use
Smoking -
*major impacts on health
*major impacts on quality of life
*much of the results are in your hands